As large parts of the world prepare for a second wave of coronavirus cases governments have pinned their hopes on the rapid development of a vaccine to provide a route out of the pandemic.
Pharmaceutical companies have moved with unprecedented speed and tens of thousands of people in more than a dozen countries — from Brazil to Saudi Arabia — have volunteered for human trials.
If the vaccines work, as early tests suggest, the button will be hit for immediate mass production at a scale and speed never seen before. But recent setbacks for at least one leading manufacturer have shown that the path to a proven and widely available shot may not be straightforward.
In total there are more than 300 vaccine candidates so far, according to the World Health Organization: roughly 40 are currently being tested on humans, and only nine of those have reached the final stage before possible implementation — Phase 3 trials.
One of the nine vaccines is being developed in the UK by AstraZeneca at Oxford university; two of the most advanced US candidates come from pharmaceutical companies Pfizer, in partnership with Germany’s BioNTech, and Moderna; four vaccines are being produced in China by Sinovac Biotech, CanSino Biologics and Sinopharm, which has two different shots in development; and one is being led by US multinational Johnson & Johnson. A Russian vaccine produced by the Gamaleya Research Institute entered Phase 3 this month. All nine have already signed purchase agreements with governments around the world.

How will the different vaccines work?
All the possible inoculations broadly follow the same logic. They deliver a protein into the body that attaches to a part of the coronavirus, called the spike, and triggers the immune system to produce antibodies and virus-fighting cells to fend off the infection.
There are dozens of possible ways to transmit immunising proteins into the body, and researchers around the world are trying different approaches.
Three of the Chinese Phase 3 candidates use an inactivated virus as their vector. In other words, Sars-Cov-2, which has been killed by heat or chemicals. In theory, it will elicit the correct immune response but without any of the severe health impacts of the live virus.
AstraZeneca, J&J, China’s CanSino and Russia’s Gamaleya Research Institute all use an adenovirus — a common virus that causes coughs and fever — that acts like a cloaked horseman, carrying the immunising protein into battle.
Moderna and Pfizer/BioNTech’s are developing an RNA-based vaccine, which uses specific parts of the Sars-Cov-2 virus’ genetic code to trigger the immune response.

How are the trials structured?
All of the Phase 3 vaccine trials are what is called “event-based”, meaning the trial only ends when a certain number of people across the vaccinated group and the control group — which receives a placebo — have contracted the virus and shown symptoms. Moderna, for example, has set the number of these so-called “positive events” at 151. It also means that the more prevalent the disease is in the population at the time of trial, the quicker it is to gather results.

While it is commonly hoped that a vaccine will completely prevent individuals from getting infected, this result is rare, and has never been achieved for other coronaviruses or strains of influenza. Instead, a more pragmatic goal, adopted by most of the vaccine developers, is the prevention of symptomatic Covid-19 infections. That is the stated objective of the AstraZeneca, Moderna, Pfizer/BioNTech and J&J vaccines.
“What we really want from a vaccine is to stop people being admitted to hospital, going to intensive care and dying,” said Andrew Pollard, who is leading the AstraZeneca trials at Oxford university. “It is likely to be a much bigger hurdle to completely prevent asymptomatic infection.”
Immunity, boosters and side-effects
Given the growing chorus of experts warning it is likely the vaccine will only confer temporary immunity, the capacity to “boost” the immune response at a later date with another shot is important.
“The assumption at the moment is that we’ll be shooting to get to a year’s immunity,” said Kate Bingham, the chair of the UK government’s Vaccine Taskforce. Many of the current vaccine candidates are designed to be taken in two doses, to increase the chance they will trigger an effective immune response.
“Even if you have a vaccine with a second dose, you may need to boost every year,” Ms Bingham said.
AstraZeneca, CanSino, J&J and the Gamaleya Research Institute all use a non-replicating viral vector — in this case an adenovirus — to deliver the vaccine to the recipient. These are infamously difficult to boost because the body learns to mount an immune response to the adenovirus and is therefore primed to fight it off quickly next time.
“It’s a potential hindrance in terms of a long term revenue stream — but one of the other vaccines could be your booster of choice,” said Matthew Harrison, a biotech analyst at Morgan Stanley.
Side effects are also being closely watched. Early trials of the Moderna vaccine for example, when participants received a dose more than double the strength of the current shot, resulted in 20 per cent experiencing significant adverse effects, including headaches and fevers.
AstraZeneca has had to pause trials twice after participants fell seriously ill and while work has resumed in the UK and elsewhere, the research remains on hold in the US.
Which countries have bought doses so far?
Despite global appeals from the WHO for states to pursue multilateral deals that provide for the equitable distribution of doses, the trials have sparked a multibillion-dollar flurry of vaccine dealmaking by national governments.
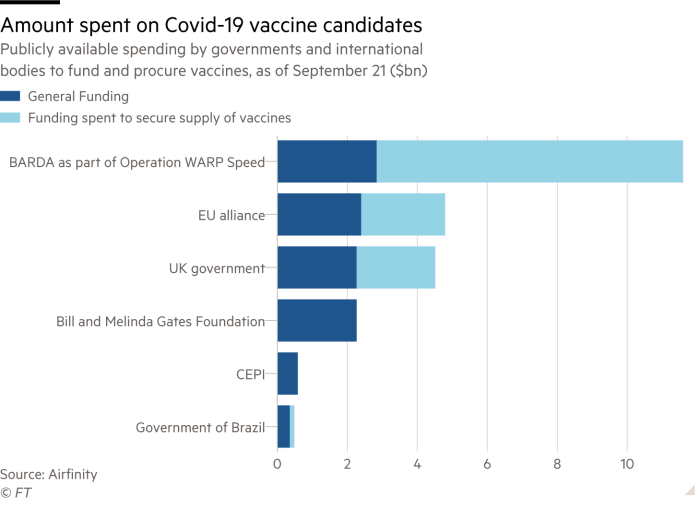
The US government’s Biomedical Advanced Research and Development Authority is the biggest spender so far, having distributed more than $10bn in funding for vaccine candidates, either via direct financing or through vaccine procurement agreements.
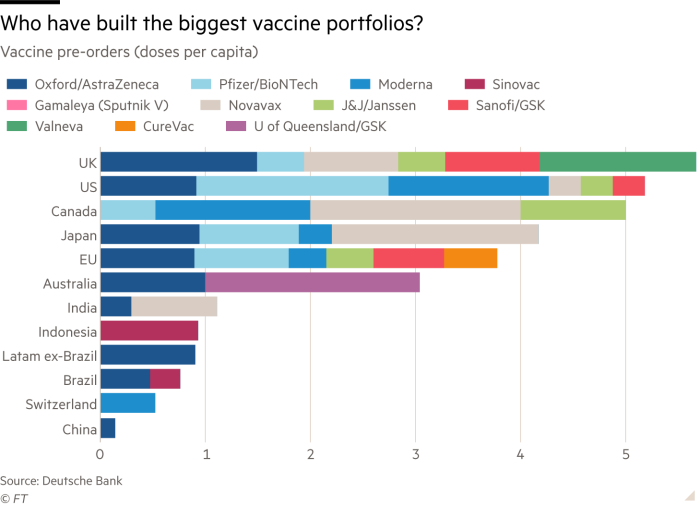
On a per-capita basis, the UK has built the largest and most diversified vaccine portfolio, according to data from Deutsche Bank, having pre-ordered more than five doses per citizen spread across six leading vaccine candidates. The UK is followed closely by the US, Canada and Japan.
In total, dealmaking by the US, UK, EU, Japan and other rich nations has meant wealthy countries representing just 13 per cent of the world’s population have bought more than half of the leading vaccine candidates’ promised doses, according to Oxfam, the charity.
Covax, the global vaccine procurement facility, designed to ensure the equitable distribution of doses, only this week secured the participation of 64 higher income countries. The Coalition for Epidemic Preparedness Innovations, one of the founders of the facility, has invested up to $895m in nine Covid-19 vaccine candidates which will be distributed under the programme.
When can we expect results?
Scientists’ forecasts for when the first vaccine could present positive Phase 3 trial results range from October this year, at the most optimistic, to mid-2021 at the most pessimistic.
Pfizer/BioNTech have said they would have sufficient data from their Phase 3 trial to begin analysis by the end of October. Moderna, which has enrolled more than 25,000 participants in its trial and given more than 10,000 of those both doses in the vaccine course, said last week that an interim analysis of trial results is more likely to begin in November and potentially as late as December.
When the AstraZeneca trial restarted in the UK in September, the company said it was still on track to submit its vaccine for regulatory approval before the end of the year. Some 18,000 individuals in the UK, US, South Africa and Brazil have received its AZD1222 vaccine as part of the trial so far.
After initial Phase 3 trial results are available, a successful vaccine could be approved by the relevant national regulator within one month, analysts estimate, allowing for the early delivery of the shot to vulnerable groups. It would likely take a further six months for full Phase 3 trial data to be collected and analysed before the shot could be made available for wider public vaccination campaigns.
Additional reporting by Hannah Kuchler and Clive Cookson
"close" - Google News
September 23, 2020 at 12:29PM
https://ift.tt/2G0OL9m
How close is a coronavirus vaccine? - Financial Times
"close" - Google News
https://ift.tt/2QTYm3D
https://ift.tt/3d2SYUY
Bagikan Berita Ini














0 Response to "How close is a coronavirus vaccine? - Financial Times"
Post a Comment